Bloating? Fix it with these 5 steps
How I help patients with normal investigations overcome persistent bloating
"I look six months pregnant!" Mrs B said, gesturing at her distended abdomen.
"And every test comes back normal."
I've heard this story countless times.
Normal bloods, normal imaging, normal endoscopy.
Yet here was someone whose quality of life was being completely derailed by relentless bloating.
After taking a detailed history - what she ate, when symptoms peaked, her bowel patterns; we embarked on a systematic five-step approach that would transform her symptoms from an 8/10 severity to barely noticeable within 12 weeks.
Today I'm sharing that exact roadmap with you...
General Disclaimer: Another Gut Group post, another disclaimer, I know, I know. If you're experiencing new bloating, you need a full history, basic investigations including blood tests (full blood count, coeliac screen, thyroid function, CA-125 (A tumour marker for Ovarian cancer (Bloating can be an initial presentation)), stool studies, and possibly imaging to rule out underlying conditions. What follows assumes you've had appropriate medical evaluation.
Step 1: Treat Constipation - Unblock the Pipe
Your gastrointestinal tract is essentially a long pipe that starts at your mouth and ends at your anus.
When that pipe gets blocked, even partially, gas has nowhere to go.
It accumulates, stretches your intestines, and creates that familiar uncomfortable distension.
Constipation is the culprit in a decent proportion of bloating cases. Even if you're having daily bowel movements, incomplete evacuation can create a traffic jam that backs everything up.
When stool sits too long in your colon, bacteria have more time to ferment undigested food particles, producing methane and hydrogen gas.
Meanwhile, the physical obstruction prevents normal gas clearance.
Bad news.
I've written extensively about this topic - check out my guide on natural constipation remedies where I detail foods like psyllium, prunes, and kiwis that can transform your bowel habits.
If diet alone doesn't work, my medical constipation treatment guide reviews what actually works (spoiler: PEG is the champion, docusate is useless).
The key is achieving complete AND satisfying bowel movements.
Start here. Seriously. Even if you don't think you're constipated.
My patient reported having daily bowel movements but admitted they felt incomplete. Addressing this was the first priority.
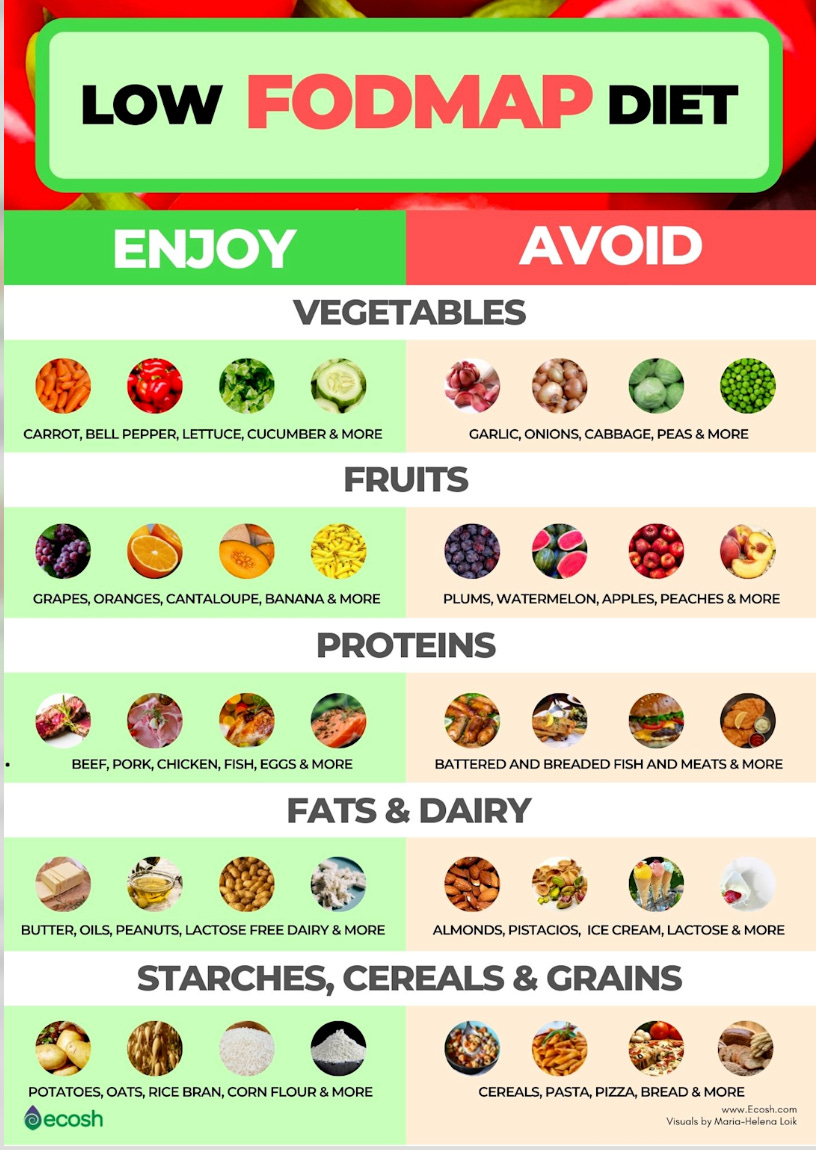
Step 2: Low FODMAP - Down the rabbit hole of Selective Elimination
I've created a comprehensive low FODMAP guide on this newsletter that walks you through the entire process step-by-step.
The key insight? You're not trying to eliminate FODMAPs forever - you're identifying which ones, and in what quantities, trigger your symptoms.
FODMAPs are carbohydrates that resist digestion in your small intestine.
High FODMAP foods draw water into your intestinal lumen through osmosis (similar to how salt makes you thirsty).
Second, your gut bacteria ferment them rapidly, producing carbon dioxide, hydrogen, and methane.
For someone with IBS or visceral hypersensitivity, this normal process becomes amplified. Your gut nerves overreact to the stretching, interpreting normal digestion as pain and discomfort.
Research from Monash University shows 75% of IBS patients experience significant improvement on a low FODMAP diet. Some studies push that number to 86% when the diet is properly supervised.
It involves 2-6 weeks of strict elimination, followed by systematic reintroduction to identify your personal triggers. Most people can eventually tolerate moderate amounts of most FODMAPs. The goal is NOT permanent restriction - it's finding your personal threshold.
Common triggers include fructans found in garlic, onions, and wheat. Mannitol lurks in cauliflower, mushrooms, and sweet potatoes.
My patient discovered that garlic and onions were major triggers, but she could tolerate most other FODMAPs in moderation. This targeted approach meant she could still enjoy most foods without fear.
Step 3: Eliminate/reduce Lactose - More Common Than You Think
70% of the world's adult population has some degree of lactase deficiency.
When you lack sufficient lactase enzyme, undigested lactose travels to your colon where anaerobic bacteria throw a fermentation party.
Carbon dioxide, hydrogen gas, organic acids, and that familiar bloated feeling about 30 minutes to 2 hours after dairy consumption.
The challenge with lactose intolerance is diagnosis. Hydrogen breath testing is considered the “gold standard”, but it has MAJOR limitations - about 6% of people produce only methane, which standard tests miss. Genetic testing exists but doesn't predict symptom severity. Many people simply don't realise they're intolerant because symptoms can be delayed and variable.
Here's my practical approach: eliminate dairy completely for two weeks, then reintroduce….bloating? You likely have lactose intolerance. Eat at your peril!
The evidence for lactase enzymes is (sort of) there. A very small crossover placebo-controlled study showed that 6,000-9,000 IU taken immediately before dairy consumption significantly reduces both symptoms and breath hydrogen levels. The enzyme (derived from Aspergillus oryzae) essentially does the work your small intestine can't. I feel stronger evidence is needed though.
Pro tip: Take it with your first bite of dairy.
Sarah was convinced she wasn't lactose intolerant because she'd "always drunk milk." Two weeks dairy-free revealed otherwise. Her bloating dropped another 20%. Now she uses lactase enzymes when she wants ice cream and sticks to hard cheeses and yogurt (naturally lower in lactose) for her daily calcium.
Step 4: Consider Gluten Elimination - But ONLY After the Above
This is where things get controversial, and I approach it with caution.
Non-coeliac gluten sensitivity is a phenomenon, but it might not be what you think. Columbia University research found that sensitive individuals show measurable immune responses - elevated antibodies against gluten and increased intestinal permeability markers that normalise on a gluten-free diet.
However, a significant portion of people who feel better gluten-free are actually responding to the reduction in FODMAPs (specifically fructans in wheat) rather than gluten itself.
Gluten can increase zonulin production, a protein that regulates intestinal permeability. This "leaky gut" phenomenon may contribute to systemic inflammation and enhanced visceral sensitivity. The theory is your gut overreacts to normal amounts of gas and fluid.
This really interesting study here found IBS patients with self-perceived gluten sensitivity reacted similarly to gluten, wheat, and sham challenges.
My recommendation: only consider eliminating gluten after you've tried the first three steps. If you do remove it, do so completely for six weeks, then re-challenge to confirm whether it's truly problematic. This should be a last resort because gluten-free diets are restrictive, expensive, and can be socially challenging.
Critical point: Always exclude coeliac disease first with proper testing while you're still eating gluten. Once you've eliminated gluten, testing becomes unreliable.
Sarah tried gluten elimination for six weeks but found no additional benefit beyond her FODMAP modifications. This saved her from unnecessary dietary restriction and the social challenges of being gluten-free.
Step 5: Targeted Therapeutics……
When dietary modifications plateau, two evidence-based options stand out.
But first, a word about SIBO (Small Intestinal Bacterial Overgrowth).
If you've tried everything and nothing works, SIBO might be the culprit. This condition, where bacteria colonise your small intestine where they shouldn't be….the bacteria ferment food before you can absorb it, creating excessive gas and bloating. Testing is not reliable but can involve breath testing or small bowel aspirate, and treatment typically requires specific antibiotics like rifaximin.
I'll be writing a comprehensive newsletter on SIBO diagnosis and treatment soon, but for now, know that persistent bloating despite all interventions warrants evaluation for SIBO.
Bifidobacterium longum 35624 has the strongest probiotic evidence for bloating. A massive meta-analysis of 72 randomised controlled trials involving 8,581 participants showed significant improvement in global IBS symptoms, including bloating. Real-world studies show 2/3rd patients achieve clinically meaningful improvement.
This specific strain modulates your microbiome composition, reduces intestinal inflammation, and actually alters gas production patterns. The key is using the right strain at the right dose: 1 billion CFU daily for at least 4-8 weeks. (note I said weeks, not days!)
Simethicone may work. This polydimethylsiloxane mixture reduces the surface tension of gas bubbles by up to 39%, allowing small bubbles to coalesce into larger ones that are more easily expelled through belching or flatulence.
A meta-analysis of 16 trials involving 5,630 patients found that people taking simethicone were 2.33 times more likely to experience bloating relief compared to placebo. The beauty is that it works locally without any systemic absorption - it's essentially inert once it does its job.
Sarah added Bifidobacterium longum after achieving partial improvement with dietary changes. Within four weeks, her residual symptoms essentially disappeared. She keeps simethicone on hand for occasional flares, particularly after restaurant meals where hidden FODMAPs might sneak in.
What Else Works?
Peppermint oil deserves an honourable mention. L-menthol blocks calcium channels in intestinal smooth muscle, preventing spasmodic contractions. A meta-analysis of 12 trials showed significant improvement with a number needed to treat of just 4 - meaning for every 4 people who try it, one will have significant improvement.
Only enteric-coated capsules work. Peppermint tea, while soothing, doesn't contain enough menthol to be therapeutic.
The gut-brain connection matters more than most people realise. Stress directly impacts gut motility and visceral sensitivity through the enteric nervous system. Diaphragmatic breathing can provide immediate relief by activating vagal tone and reducing sympathetic overdrive.
Movement is medicine. Even gentle walking stimulates peristalsis and helps trapped gas migrate through your system. Think of it as manually pumping your intestinal pipes. Read my workout out guide here
Mrs B’s Transformation
Twelve weeks after our first consultation, Mrs B’s bloating had reduced from an 8/10 to a 2/10.
She could wear fitted clothes comfortably again. Restaurant meals no longer required strategic planning. Most importantly, she'd stopped structuring her entire life around her symptoms.
The transformation came from methodically working through each step:
Weeks 1-2: Optimising bowel movements with psyllium and adequate hydration
Weeks 3-6: Low FODMAP elimination, identifying garlic and onions as major triggers
Weeks 7-8: Lactose elimination trial, confirming moderate intolerance
Week 9: Skipped gluten elimination after adequate improvement
Weeks 10-12: Added Bifidobacterium longum, achieving near-complete resolution
Not everyone needs all five steps. Start with constipation management and low FODMAP, then add interventions based on your response. Give each change at least 2-4 weeks….your gut doesn't adapt overnight.
That’s my bloating guide!
Bloating is a symptom with identifiable triggers and evidence-based solutions.
The key is systematic investigation and a structured management plan.
Work through these steps methodically, keep a detailed symptom diary, and give each intervention adequate time.
Most importantly, remember that bloating is your body's way of communicating that something needs attention. Listen to it, work with it, and you can find relief.
Have you tried any of these approaches? What worked for you? I'd love to hear about your experience in the comments.
Stay comfortable, friends!
P.S. If you're struggling with bloating despite these interventions, or if you have any red flag symptoms (unintentional weight loss, blood in stool, persistent pain, onset after age 50), please see your doctor urgently. Sometimes bloating signals something that needs immediate medical attention.
Struggling with liver or digestive issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
References
Vasant DH et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut. 2021;70(7):1214-1240
Marsh A, Eslick EM, Eslick GD. Does a diet low in FODMAPs reduce symptoms associated with functional gastrointestinal disorders? A comprehensive systematic review and meta-analysis. Eur J Nutr. 2016;55(3):897-906
Staudacher HM et al. A Diet Low in FODMAPs Reduces Symptoms of Irritable Bowel Syndrome as well as Traditional Dietary Advice: A Randomized Controlled Trial. Gastroenterology. 2017;153(4):936-947
Ibarra A et al. Effect of lactase on symptoms and hydrogen breath levels in lactose intolerance: A crossover placebo-controlled study. United European Gastroenterol J. 2021;9(1):76-84
Uhde M et al. Intestinal cell damage and systemic immune activation in individuals reporting sensitivity to wheat in the absence of coeliac disease. Gut. 2016;65(12):1930-1939
McFarland LV et al. Strain-specific and outcome-specific efficacy of probiotics for irritable bowel syndrome: A systematic review and meta-analysis. EClinicalMedicine. 2021;41:101154
Yuan F et al. Effect of Bifidobacterium longum 35624 on disease severity and quality of life in patients with irritable bowel syndrome. World J Gastroenterol. 2022;28(7):732-744
Zhang L et al. Simethicone decreases bloating and improves bowel preparation effectiveness: a systematic review and meta-analysis. Surg Endosc. 2019;33(12):3899-3909
Weerts ZZRM et al. Efficacy and Safety of Peppermint Oil in a Randomized, Double-Blind Trial of Patients With Irritable Bowel Syndrome. Gastroenterology. 2020;158(1):123-136
Mari A et al. Bloating and Abdominal Distension: Clinical Approach and Management. Adv Ther. 2019;36(5):1075-1084
General Disclaimer
Please note that the opinions expressed here are those of Dr Hussenbux and do not necessarily reflect the positions of Buckinghamhsire Healthcare NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.






Nice! Thank you. I look forward to your SIBO article.
Really helpful breakdown, #3 and #5 caught me off guard. Didn’t realize lactose and targeted probiotics could have that much impact. Useful as always!