SIBO - When Bowel Bacteria Become Bad
Stolen B12 and the the recent research... my deep dive
Mr Z sat opposite me…exhausted.
One year of bloating, brain fog, and that peculiar pattern…feeling worse after "healthy" meals, better after fasting.
His B12 was mysteriously low despite eating meat.
Classic Small Intestinal Bacterial Overgrowth (SIBO)?
Six weeks later, after rifaximin and some strategic dietary shifts, he messaged me:
"I forgot what normal felt like."
Let’s dive in!
What SIBO actually is
Small Intestinal Bacterial Overgrowth sounds complex. It is and it is not.
Your small intestine should be relatively sterile…think exclusive nightclub, not crowded pub.
Normal bacterial counts stay below 10,000 per millilitre. In SIBO, colonic bacteria gate-crash upward, multiplying past 100,000.
Party's over. Digestion derails.
The latest research reveals three distinct types.
Hydrogen-dominant SIBO brings diarrhoea and urgency
Methane-dominant (technically IMO - Intestinal Methanogen Overgrowth) causes constipation which can be stubborn
Hydrogen sulphide, the newest member, smells exactly how you'd imagine.
How common? Difficult to say as the diagnosis is tricky (more on this later).
Hit 75? Your risk increases. Have inflammatory bowel disease? Your odds jump.
2024 brought some important research. Major gastroenterology societies now question whether SIBO exists as commonly diagnosed. They've essentially said: "We've been wrong about breath testing." At. Long. Last!
However…the condition remains real for those who have it.
Causes and the nutrition connection
SIBO doesn't just happen. Something breaks first.
Your stomach acid acts like a bouncer, killing incoming bacteria.
Proton pump inhibitors neutralise that bouncer. More on this here
The migrating motor complex - your gut's cleaning wave between meals - sweeps bacteria downstream.
Diabetes, scleroderma, or previous surgery can silence these waves. Bacteria accumulate. Problems begin.
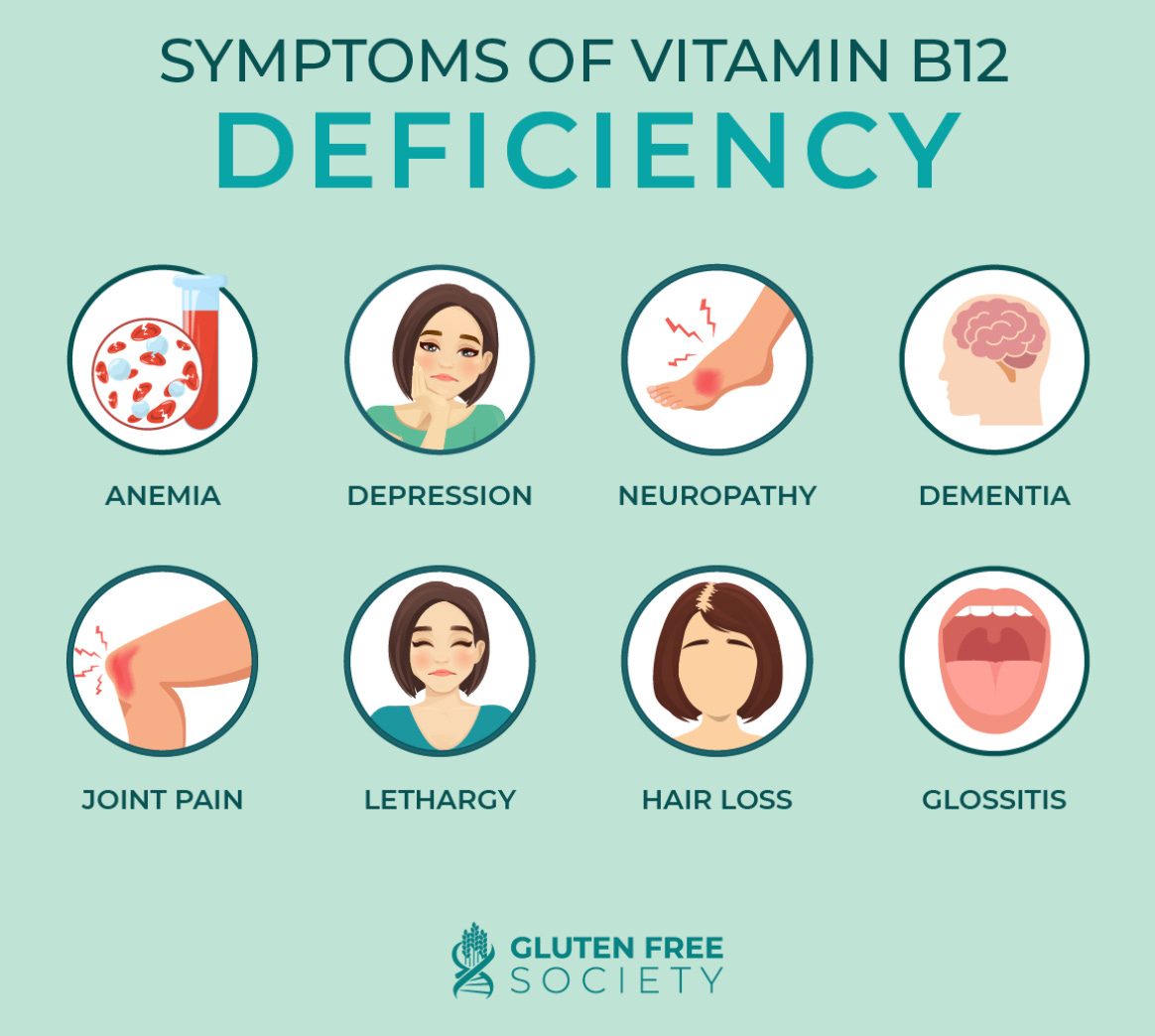
The B12 mystery makes perfect sense once you understand bacterial competition. Those uninvited bacteria bind B12 before you can absorb it. Studies show Proteus and Klebsiella steal over 50% of available B12. Hydrogen-producers are the worst thieves.
The extra bacteria actually make folate. SIBO patients often show the peculiar pattern of low B12, normal or high folate. It's diagnostic gold for me…
Fat-soluble vitamins disappear too. Excess bacteria break down bile salts prematurely, sabotaging fat absorption. Vitamins A, D, E, K - all casualties.
The diagnostic dilemma
Breath tests dominated SIBO diagnosis for twenty years. You drink sugar water, breathe into tubes, measure hydrogen and methane.
Simple? Sure. Accurate? That's the problem.
2024's bombshell research showed glucose breath tests achieve only 55% sensitivity. Flip a coin.
Lactulose tests? Worse - 42% sensitivity.
The fundamental flaw: these tests measure transit time, not bacterial location. Fast transit creates false positives. Slow transit misses real cases.
Some beneficial bacteria produce hydrogen. Some pathogens don't. The test's basic premise crumbles under scrutiny.
Duodenal aspiration….doing a gastroscopy and sampling small intestine fluid remains the "gold standard."
But it's invasive, expensive, often unavailable. Even then, 20% contamination rates and inability to culture most gut bacteria limit accuracy.
The latest European and American guidelines?
"Abandon routine breath testing for SIBO."
Twenty years of practice, overturned.
So what now?
Treat symptoms empirically. Test only high-risk patients.
Sometimes clinical judgment trumps imperfect tests.
Treatment options?
Rifaximin leads the evidence base. This antibiotic barely absorbs…less than 0.4% enters your bloodstream. It stays local, nuking small intestinal bacteria while sparing the colon. Studies show 71% eradication rates at proper doses.
Combine this with elemental diets. Pre-digested nutrients absorbed high in the intestine, starving downstream bacteria. Success rates hit 85% at three weeks. Challenging? Absolutely. Effective? Remarkably.
For methane-dominant SIBO, rifaximin alone may not succeed. Add neomycin. Success jumps up. Metronidazole works too, particularly for stubborn methane producers.
Dietary approaches help symptoms but don't cure SIBO.
Low FODMAP reduces fermentable sugars, calming symptoms within days. Use it strategically during treatment, not forever. Long-term restriction harms your microbiome.
Probiotics? Complicated.
Meta-analyses shows some improvement with specific strains like Saccharomyces boulardii.
However, recent probiotic use associates with positive methane breath tests. Some practitioners avoid them entirely during active treatment.
Rebuilding after antibiotics
Here's what UCLA research revealed: fermented foods beat probiotic supplements for microbiome restoration.
Skip the pills. Embrace the plate.
Kefir, kimchi, sauerkraut, proper yogurt - these living foods gently recolonise your gut. Their diverse microbial communities outperform single-strain supplements. Start slowly. A tablespoon of sauerkraut. A small glass of kefir. Build gradually.
Don't rush probiotics immediately post-antibiotics. Feed the good bacteria first - resistant starch from cooled potatoes, prebiotic fibres from artichokes, polyphenols from berries. Let your native bacteria recover.
Read my nutrition cheat sheet here
The microbiome typically rebounds within 1-2 months. Unless you've had multiple antibiotic courses. Then recovery stretches longer, sometimes incompletely.
The evolving picture
The 2024 SIBO research raised relevant questions.
Are we overdiagnosing? Overtreating? The answer: probably, sometimes.
Yet for true SIBO patients - post-surgical, scleroderma, small bowel diverticulosis, severe motility disorders - the condition remains devastatingly real.
New connections emerge constantly. SIBO associates with metabolic liver disease. With rosacea. With restless legs. The small intestine influences more than we imagined.
What do we really need?
Molecular diagnostics that identify specific bacterial signatures. Personalised treatment based on your unique dysbiosis. But we're not there yet.
For now, remember this: SIBO exists on a spectrum. Severe cases need aggressive treatment. Mild cases might resolve with simple dietary changes. Most fall somewhere between.
Trust symptoms over tests. If rifaximin helps but doesn't cure, try combinations. If antibiotics fail, consider elemental diets. Always rebuild deliberately afterward.
Mr Z’s case wasn't unusual. Just under-treated for too long. Sometimes the simplest explanation - bacteria in the wrong place - really is the answer.
Struggling with liver or digestive issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
References
Kashyap PC, et al. Critical appraisal of the SIBO hypothesis and breath testing. Neurogastroenterology & Motility. 2024;36(6):e14817.
Leite G, et al. Defining Small Intestinal Bacterial Overgrowth by Culture and High Throughput Sequencing. Clinical Gastroenterology and Hepatology. 2023;21(9):2341-2349.
Gatta L, Scarpignato C. Systematic review with meta-analysis: rifaximin is effective and safe for the treatment of small intestine bacterial overgrowth. Alimentary Pharmacology & Therapeutics. 2017;45(5):604-616.
Pimentel M, et al. A 14-day elemental diet is highly effective in normalizing the lactulose breath test. Digestive Diseases and Sciences. 2004;49(1):73-77.
Villanueva-Millan MJ, et al. Do Herbal Supplements and Probiotics Complement Antibiotics and Diet in the Management of SIBO? A Randomized Clinical Trial. Nutrients. 2024;16(7):1083.
Zhong C, et al. Probiotics for Preventing and Treating Small Intestinal Bacterial Overgrowth. Journal of Clinical Gastroenterology. 2017;51(4):300-311.
Gandhi A, et al. Methanogens and Hydrogen Sulfide Producing Bacteria Guide Distinct Gut Microbe Profiles and Irritable Bowel Syndrome Subtypes. The American Journal of Gastroenterology. 2022;117(12):2055-2066.
Wijarnpreecha K, et al. Small intestinal bacterial overgrowth and metabolic dysfunction-associated steatotic liver disease. World Journal of Hepatology. 2024;16(12):1458-1467.
General Disclaimer
Please note that the opinions expressed here are those of Dr Hussenbux and do not necessarily reflect the positions of Buckinghamhsire Healthcare NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.






Very well done! On the prescriber's side, rifaximin is often cost prohibitive. The patient with an elevated folate and low B12 is a classic SIBO board question!
Agree with a lot of what you said here, especially the effectiveness of rifaxamin + low fodmap via the starve it out method, and pushing for probiotics through food rather than supplementing.
When you mentioned treating suspected SIBO instead of confirming through breath testing, my main concern is rifaxamin is a very expensive antibiotic. Most insurance companies won’t cover without a dx, and even so, sometimes make you try and fail with other abx first. How do you navigate or justify the cost for your patients in these cases without a dx?