A Gastroenterologists secrets to treating reflux
This plus last weeks article - game changer for reflux
So you checked out last weeks article...
And you still have reflux???
I need to pull out all the stops now.
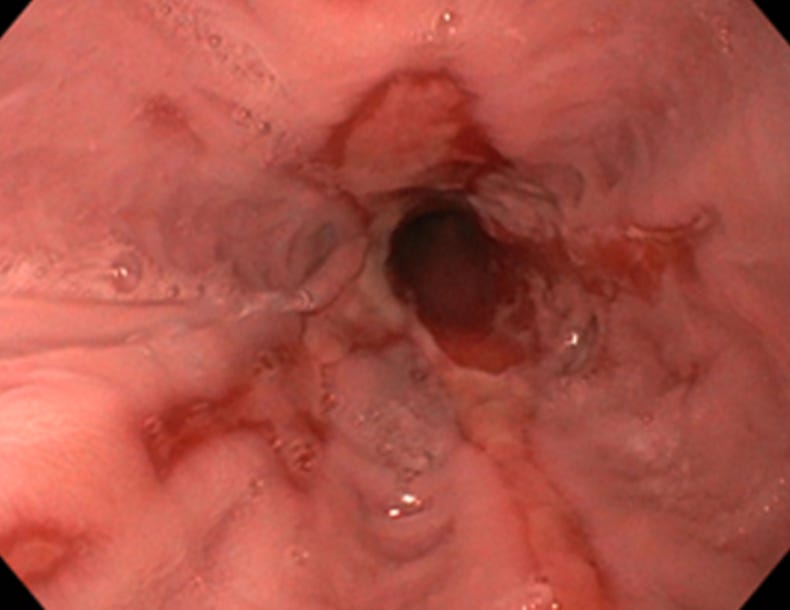
Once and for all….this is how I manage reflux medically in patients with normal gastroscopies.
Disclaimer: If you have persistent reflux symptoms, alarm features (difficulty swallowing, unintentional weight loss, vomiting blood), or symptoms lasting more than a few weeks, you need urgent investigation with gastroscopy +/- more. Don’t wait.
If you suffer from reflux PLEASE read this article first before continuing!
1. Gaviscon: you’re probably using it wrong
Most people treat Gaviscon like any old antacid. Swallow it whenever. Before food, after food, doesn’t matter.
It kind of matters.
Gaviscon contains two active components working in beautiful harmony.
Sodium bicarbonate neutralises stomach acid on contact.
Sodium alginate (derived from seaweed) reacts with that acid to form a viscous gel.
This gel floats on top of your stomach contents like a protective raft.
After you eat, your stomach produces fresh acid that layers on top of your meal rather than mixing with it. This creates what gastroenterologists call the “acid pocket”, an unbuffered, highly acidic zone sitting right near your oesophageal junction.
It’s the primary source of postprandial reflux. The acid pocket can persist for 90-120 minutes after eating.
Gaviscon’s alginate raft physically floats into this acid pocket. Scintigraphy studies have visualised this co-localisation in real patients. One study found the raft reduced reflux events from 15 to just 3.5, with the time to first acid reflux increasing to over an hour.
The practical takeaway: Take Gaviscon after meals, not before. Taking it before eating means food passing through will disrupt the protective raft before it can do its job. Gaviscon® Chew tablets thoroughly. Stay upright for 30 minutes. The raft remains protective for up to four hours.
I do love this advert!
2. Mediterranean diet and alkaline water: the drug-free approach
A 2017 study published in JAMA Otolaryngology compared two approaches for treating laryngopharyngeal reflux (LPR), that irritating cousin of heartburn that affects the throat and voice box.
The first group received standard treatment: twice-daily proton pump inhibitors plus dietary precautions. The second group? No medication. Instead, they drank alkaline water (pH above 8.0) and followed a 90-95% plant-based Mediterranean-style diet.
62.6% of the dietary group achieved clinically meaningful improvement, compared to 54.1% on PPIs.
Not statistically different but the percent reduction in symptom scores was significantly greater in the diet group: 39.8% versus 27.2%.
The theory behind this approach involves pepsin, the digestive enzyme that causes much of the damage in reflux. Pepsin remains active up to pH 8.0. Alkaline water may help inactivate it. Meanwhile, a plant-based diet reduces gastric amino acid load, potentially decreasing both gastrin secretion and pepsin activity.
Caveats: This was a retrospective study with significant limitations. We can’t distinguish whether the benefit came from alkaline water, the Mediterranean diet, or both. But for patients seeking non-pharmacological options, particularly those concerned about long-term PPI use, it offers a genuine, evidence-based alternative worth trying.
Plus there is no harm with this approach.
Double plus….mediterranean diet has so many crossover benefits with brain, heart and liver health.
3. Neobianacid: the mucosal protector
I’ll admit, when I first heard about this product, I was sceptical. Another “natural” remedy? Oh dear….
Then I read the trial.
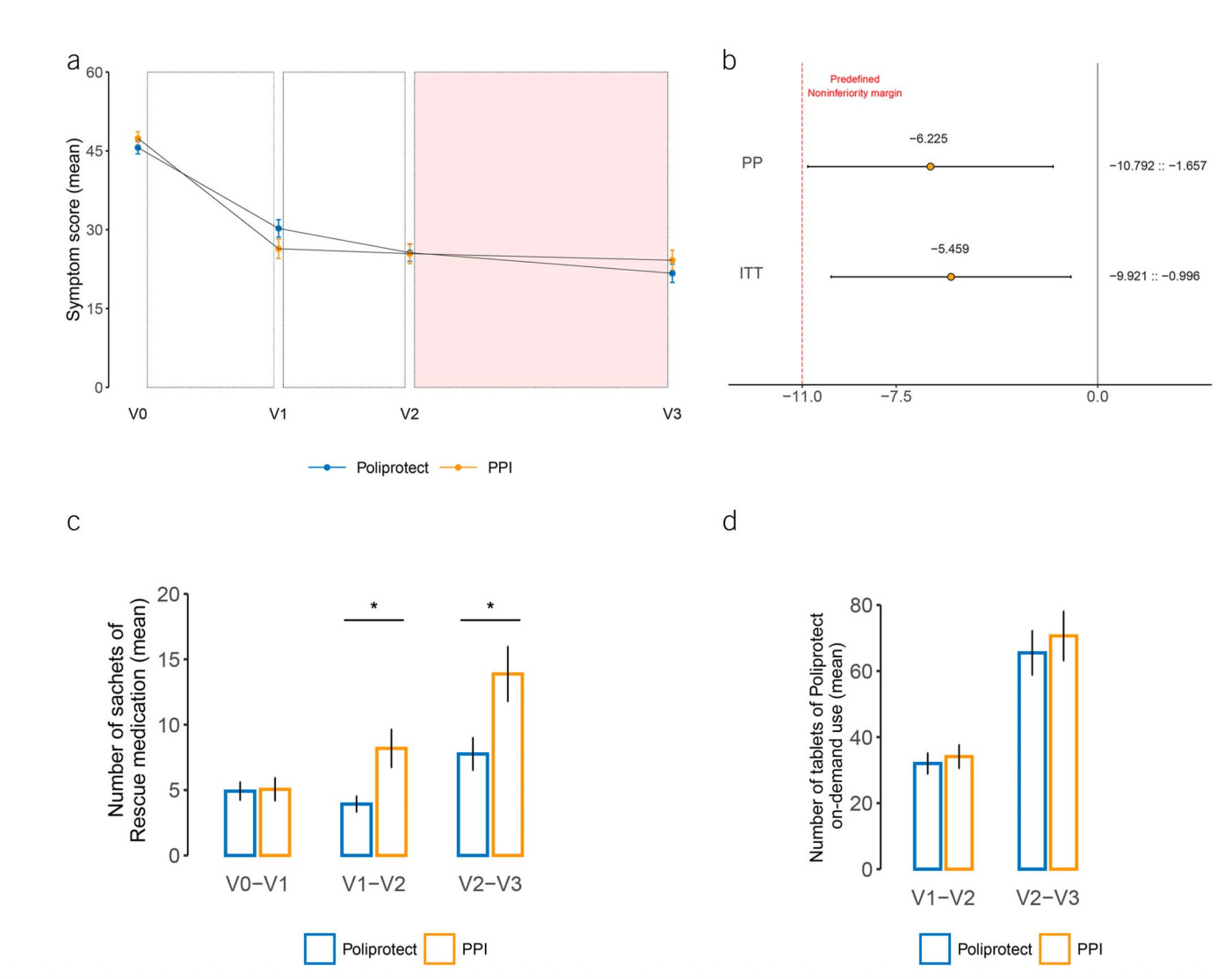
A 2023 randomised controlled trial published in the American Journal of Gastroenterology compared Neobianacid (marketed as Poliprotect) head-to-head against omeprazole 20mg daily in 257 patients with heartburn and epigastric pain. These weren’t patients with severe erosive disease; they had negative endoscopies but persistent symptoms.
Neobianacid was non-inferior to omeprazole for symptom relief at two weeks.
By day 28 and beyond, symptom scores were virtually identical between groups.
The Neobianacid group required significantly less rescue medication. And unlike PPIs, it caused no changes to gut microbiome composition; whereas the omeprazole group showed enrichment of oral bacteria in the gut, a pattern we increasingly associate with PPI use.
How does it work? The active ingredients include high-molecular-weight polysaccharides from aloe vera, mallow, and marshmallow root, combined with natural limestone and sodium bicarbonate.
These form a mucoadhesive film that physically coats and protects the oesophageal and gastric lining.
Flavonoids from chamomile and liquorice provide antioxidant effects.
It’s a barrier-forming approach rather than acid-suppressing. The polysaccharides become more adhesive in acidic conditions, precisely where you need them most.
Bottom line: For moderate, non-erosive symptoms, Neobianacid offers a legitimate PPI alternative. Particularly valuable for patients who want to avoid or step down from acid suppression.
If no improvement after 30 days….just stop it!
4. The IQoro device: training your swallowing muscles (weak evidence)
This one I’m on the fence.
IQoro is a neuromuscular training device, essentially a small curved plate that sits between your teeth and lips. You pull against it for 5-10 seconds while pressing your lips firmly together. Three pulls, three times daily. Total training time: 90 seconds.
The mechanism? When you pull, sensory signals travel via neural pathways to the brain, activating motor responses in approximately 148 muscles from your lips down to your diaphragm.
High-resolution manometry studies demonstrate that IQoro traction increases pressure in the diaphragmatic hiatus region from 0 mmHg at rest to 65 mmHg.
This strengthens the muscular fibres that normally compress the oesophagus like a pinch-cock valve, helping prevent reflux.
A 2015 study in the World Journal of Gastroenterology followed 43 adults with long-standing swallowing difficulties and reflux symptoms through 6-8 months of IQoro training. Of those with reflux symptoms, 100% showed improvement. Other studies in patients with verified hiatus hernia demonstrated similar benefits regardless of BMI.
The honest picture: The evidence base remains limited.
Most studies are small, without control groups, and the device’s inventor co-authored many of them.
IQoro was listed in the NHS Drug Tariff in 2022 at £121, IQoro but NICE has not issued formal guidance recommending it, citing insufficient evidence for a full health technology evaluation. Some regional NHS bodies have advised against routine prescription pending further high-quality trials.
That said, for patients with mild-to-moderate reflux who prefer avoiding medications and are willing to commit to months of daily training, it represents an interesting option. The safety profile is excellent.
The worst that happens is it doesn’t work.
I personally don’t recommend this. Sometimes its patient led with variable responses.
Speak to your specialist first before considering this.
5. Omeprazole: the reliable workhorse
Sometimes you just need to suppress the acid.
Omeprazole belongs to the proton pump inhibitor (PPI) family. It works by irreversibly binding to hydrogen-potassium ATPase enzymes in stomach parietal cells; the “proton pumps” responsible for secreting gastric acid. Block these pumps, and acid production drops dramatically. The effect persists for up to 48 hours even though the drug itself is eliminated within hours.
For erosive oesophagitis, peptic ulcers, and severe GORD, PPIs remain the gold standard. They heal damaged tissue. They provide reliable symptom control. They work.
The caveat: Long-term use carries risks. Research has associated chronic PPI therapy with osteoporosis, small intestinal bacterial overgrowth and micronutrient deficiencies. There’s also the issue of hypochlorhydria (too little stomach acid) leading to impaired nutrient absorption and potential bacterial overgrowth.
I’ve written previously about why I encourage patients to use PPIs responsibly here. They’re brilliant tools. But tools, not indefinite solutions.
If you’re on omeprazole long-term and wondering whether you still need it, speak to your doctor about a trial reduction. Often, combining a step-down approach with the treatments above allows successful de-prescribing.
The path forward
Reflux is rarely one-size-fits-all.
Some patients need aggressive acid suppression during healing phases. Others do beautifully with lifestyle changes and barrier-forming agents. Many benefit from combinations; perhaps Gaviscon after meals alongside dietary modifications, sensible dietary changes while tapering PPIs.
The goal isn’t eliminating stomach acid entirely. You need it. For digestion. For killing pathogens. For absorbing nutrients.
The goal is keeping it where it belongs.
Armed with these options, you and your healthcare provider can find the approach that works for your specific situation.
Struggling with liver or digestive issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/ (I offer video and face to face consultations)
References
Kwiatek MA, et al. An alginate-antacid formulation (Gaviscon Double Action Liquid) can eliminate or displace the postprandial ‘acid pocket’ in symptomatic GERD patients. Aliment Pharmacol Ther. 2011;34(1):59-66.
Rohof WO, et al. An alginate-antacid formulation localizes to the acid pocket to reduce acid reflux in patients with gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2013;11(12):1585-91.
Zalvan CH, et al. A Comparison of Alkaline Water and Mediterranean Diet vs Proton Pump Inhibition for Treatment of Laryngopharyngeal Reflux. JAMA Otolaryngol Head Neck Surg. 2017;143(10):1023-1029.
Corazziari ES, et al. Poliprotect vs Omeprazole in the Relief of Heartburn, Epigastric Pain, and Burning in Patients Without Erosive Esophagitis and Gastroduodenal Lesions: A Randomized, Controlled Trial. Am J Gastroenterol. 2023;118(11):2014-2024.
Hägg M, et al. Esophageal dysphagia and reflux symptoms before and after oral IQoro training. World J Gastroenterol. 2015;21(24):7558-7562.
De Ruigh A, et al. Gaviscon Double Action Liquid (antacid \u0026 alginate) is more effective than antacid in controlling post-prandial oesophageal acid exposure in GERD patients. Aliment Pharmacol Ther. 2014;40(5):531-7.
General Disclaimer
Please note that the opinions expressed here are those of Dr Hussenbux and do not necessarily reflect the positions of Buckinghamshire Healthcare NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.




A few years ago my persistent cough turned out to be caused by reflux. I hadn’t had any heartburn, but often coughed a lot in the mornings. The clever doctor, after checking my lungs etc of course, prescribed Somac (Pantoprazol) and soon the differential diagnosis was obvious! But as the medication trial was done, I also got myself a wedge pillow - and started intermittent fasting, which I had already planned for some time. Well, it became my lifestyle. Already during the first year I lost over 10 kilograms, and since I stopped late-night eating and snacking, I have had no more symptoms. Of course, sometimes I ”choose to” take the risk on some special occasions like dinner parties (also alcohol is a significant factor), and a couple of times I have indeed regretted not having any Gaviscon in stock! Normally I never take any antacids, but I guess I should have some at home just in case…! But in general: wedge pillow, mainly no food or drink other than water after about 6pm, and as a last resort after a stupid late(ish) snack: sleeping on my left side! Really, left side sleeping works like magic ”if all else fails”.😄 Anyway, my main point here is that the unnatural habit of constant late-night eating can make some of us feel very sick, not knowing the reason.
Thanks again for all the education! Can I just ask, you mention Gaviscon, but are Rennie tablets as effective as the liquid Gaviscon? Thanks.