The Bug That Changed Everything We Knew About Stomach Problems
For decades, doctors told patients with stomach ulcers the same thing: reduce your stress, cut back on spicy food, and take some antacids.....until 1984
“Just take some omeprazole”….
Sadly, even after 6 weeks of regular use, the reflux and abdominal pain persisted.
“Cut down on the spicy food and citrus”.
Despite going on a very bland diet the symptoms refused to budge…
This was the frustrating cycle patients endured before 1984, when two Australian doctors made a discovery so extraordinary that one had to poison himself to prove it.
The Doctor Who Drank Bacteria to Prove a Point
Barry Marshall was frustrated.
He and his colleague Robin Warren had found strange spiral-shaped bacteria living in the stomachs of patients with gastritis and ulcers.
But when they tried to tell the medical community that these bacteria and not stress or diet, were causing stomach problems…nobody believed them.
After all, everyone "knew" that nothing could survive in the acidic environment of the stomach.
So Marshall did something that would make him either a medical hero or a cautionary tale: he drank a vial of the bacteria.
Within days, he developed gastritis. His stomach lining became inflamed, he felt nauseated, and his breath smelled terrible.
But he had proven his point…
The bacteria, which we now call Helicobacter pylori or H. pylori for short, could indeed cause stomach disease.
Follow-up endoscopy revealed severe active gastritis with inflammatory cell infiltration, proving that H. pylori was indeed a pathogen capable of causing disease in healthy individuals
In 2005, Marshall and Warren were awarded the Nobel Prize in Physiology or Medicine, with the Nobel Committee stating that their discovery transformed peptic ulcer disease "from a chronic, frequently disabling condition, to a disease that can be cured by a short regimen of antibiotics"
The global prevalence…
Here's something that might surprise you.
Nearly half the world's population carries H. pylori in their stomachs right now.
But the story gets more interesting when you look at where it thrives most.
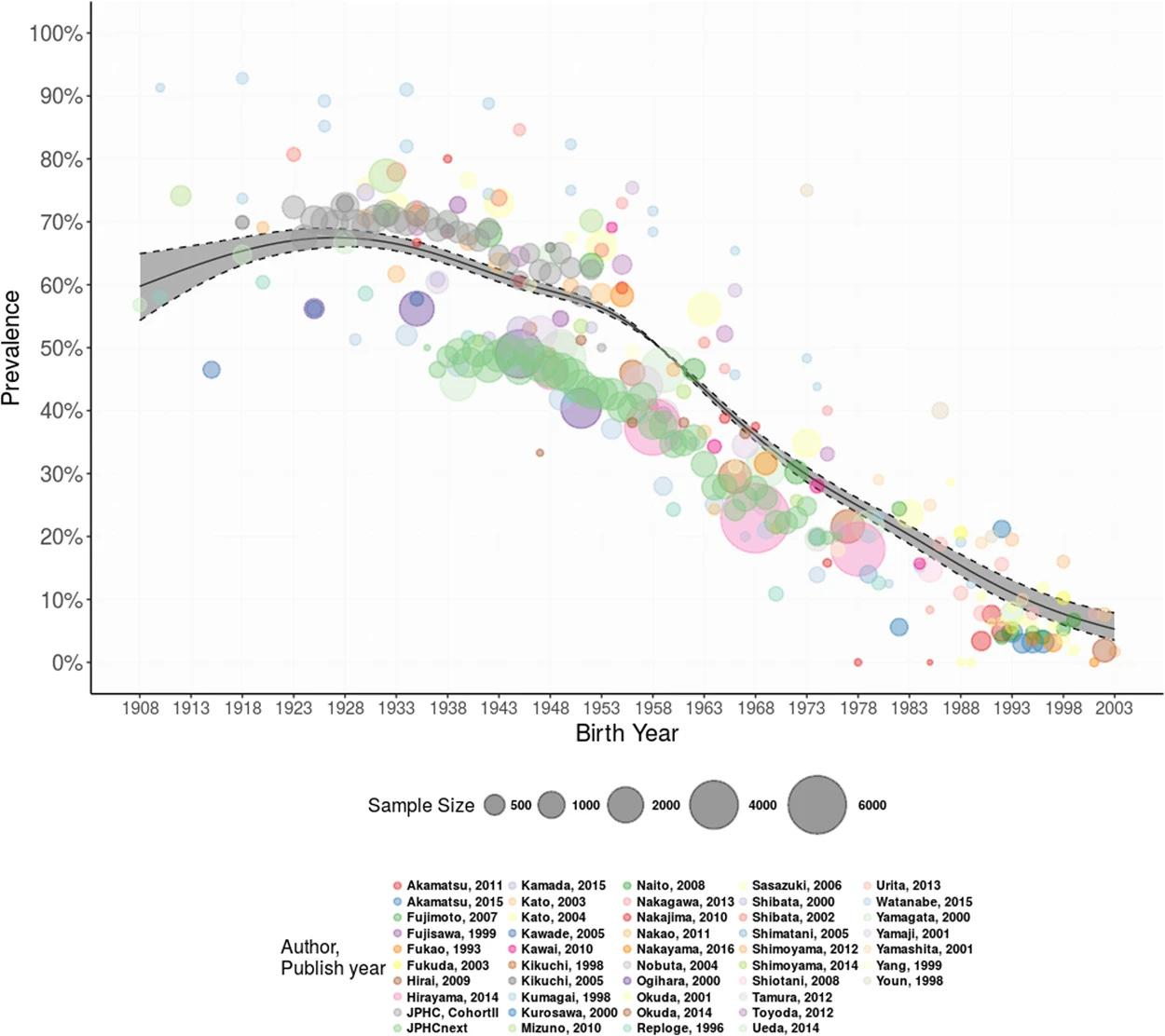
In parts of Africa, up to 70% of adults harbour these bacteria. In Latin America, the rates hover between 57% and 63%. Meanwhile, in developed nations, we're seeing a dramatic decline. Japan, for instance, has watched infection rates plummet from 73% in 1974 to just 19% in 2019.
The secret? Better sanitation, cleaner water, and less crowded living conditions.
This bacteria spreads the way many infections do…through contaminated water, food, or close contact with infected individuals.
It's particularly fond of crowded households where hygiene infrastructure might be lacking. In fact, many people pick up H. pylori as children and carry it silently for decades.
Silently sitting in your stomach
Here's where things get tricky: most people with H. pylori have no idea they're infected. The bacteria can live peacefully in your stomach for years without causing any problems. But for about 10-15% of carriers, symptoms can develop.
When H. pylori decides to act up, it can cause burning stomach pain that feels worse when your stomach is empty. You might feel bloated after meals, experience unexpected nausea, or find yourself feeling full after eating just a small amount.
In severe cases, people might vomit blood or notice their stools turning black (melaena) both signs that require immediate medical attention.
Why Your Antacids Might Be Hiding the Problem
If you have been taking proton pump inhibitors (PPIs) like omeprazole for heartburn, you might be inadvertently hiding the H. pylori. These medications, while excellent at reducing stomach acid, can suppress the bacteria just enough to cause false negative test results. Studies show that PPIs can lead to incorrect test results in 33-56% of cases.
This creates a frustrating scenario: you might have the infection, but your test says you don't. That's why your gastroenterologist may recommend stopping PPIs for at least two weeks before testing for H. pylori…though always consult your physician before changing any medications.

H.Pylori and Stomach Cancer
Here's the sobering part: H. pylori is the leading cause of stomach cancer worldwide. The bacteria doesn't cause cancer overnight, though. It's more like a slow-motion domino effect that scientists call the "Correa Cascade."
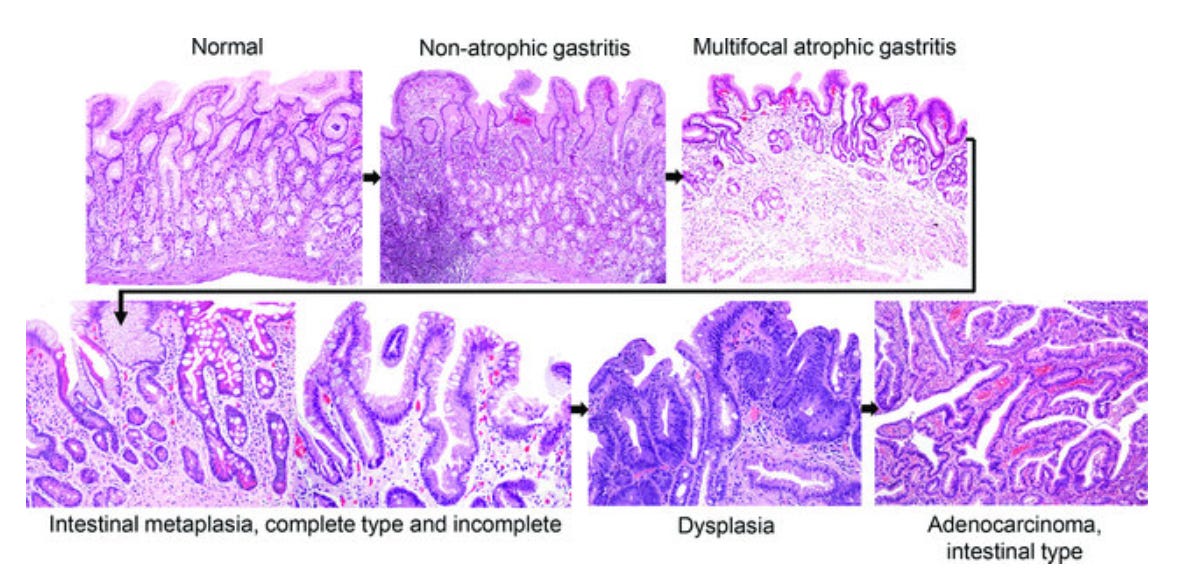
First, the bacteria causes chronic inflammation in your stomach lining. Over years or decades, this inflammation can lead to atrophic gastritis, where your stomach loses its ability to produce acid properly. Some areas might then undergo intestinal metaplasia…essentially, your stomach cells start looking more like intestinal cells. From there, dysplasia can develop, and eventually, in some cases, cancer.
The good news? This process typically takes decades, and treating the infection can stop it in its tracks. Studies show that eliminating H. pylori reduces stomach cancer risk by about 50%. The key is catching and treating it before significant damage occurs.

Testing: Getting it right through non-invasive measures first
There are several ways to test for H. pylori, each with its own pros and cons.
The urea breath test is popular because it's non-invasive. You simply drink a special solution and breathe into a bag. The bacteria's enzyme activity changes your breath composition, revealing its presence.
There's also a stool antigen test that looks for bacterial proteins
Blood tests can confirm antibodies to H. Pylori, however, are unable to distinguish between current or past infection.
For those already getting an endoscopy (gastroscopy), doctors can take biopsies to examine directly.
But here's a crucial detail many doctors miss: proper diagnosis requires multiple biopsies from different parts of the stomach. The Sydney System recommends five specific locations. This matters because H. pylori can hide in patches, especially in older patients or those with advanced stomach damage.

Treatment: Triple eradication therapy
Once diagnosed, treatment typically involves a combination of antibiotics and acid-suppressing medications. The standard "triple therapy" includes a PPI plus amoxicillin and clarithromycin, which works about 85-90% of the time.
For those allergic to penicillin, alternative combinations using tetracycline or newer acid suppressors like vonoprazan show promising results. Most hospitals use a regional or national guideline for antibiotic therapy.
The challenge? Antibiotic resistance is rising. In some regions, up to half of H. pylori strains resist clarithromycin, one of our main weapons against the bacteria. This has led to more complex "quadruple therapy" regimens that add bismuth (yes, the same ingredient in Pepto-Bismol) to improve success rates.
if your gastroscopy does show features of severe atrophy or gastric intestinal metaplasia you are eligible for surveillance to ensure there is no further progression of stomach damage / correa cascade.
Who Should Get Tested?
You should definitely consider it if you have persistent stomach symptoms, a personal history of ulcers, or a family history of stomach cancer. Some experts also recommend testing for people with unexplained iron deficiency anaemia or certain autoimmune conditions.
In regions with high stomach cancer rates, some countries have implemented population-wide screening programs. Japan, for instance, offers H. pylori testing to all residents, contributing to their declining infection and cancer rates.
The Bigger Picture: A Preventable Tragedy
What strikes me most about the H. pylori story is how it represents both a massive public health success and an ongoing challenge. We have gone from not knowing this bacteria existed to understanding its role in everything from ulcers to cancer. We have effective treatments, yet millions still suffer from preventable H. pylori-related diseases.
The discovery also reminds us to question medical dogma. For decades, the brightest minds in medicine were certain that bacteria couldn't survive in stomach acid. It took two persistent researchers and one very brave self-experiment to prove otherwise. Their initial claims were widely dismissed, however now they are Nobel prize winners!
What You Can Do
If you're experiencing persistent stomach problems, don't just reach for antacids and assume it's stress. Talk to your doctor about H. pylori testing, especially if you have risk factors. Remember to mention any acid-suppressing medications you're taking, as these can affect test results. The initial screening tests are simple and non-invasive.
For those diagnosed with H. pylori, take the full course of antibiotics as prescribed, even if you feel better halfway through. Incomplete treatment contributes to antibiotic resistance and treatment failure.
Most importantly, don't panic! While H. pylori can cause serious problems, it's also one of the most treatable infections we know of.
The story of H. pylori teaches us that sometimes our biggest health threats come in the smallest packages. But it also shows us that with curiosity, courage, and good science, we can tackle even the most entrenched medical mysteries. After all, if two doctors from Perth could overturn a century of medical wisdom with some bacteria and a brave gulp, imagine what other health revelations await discovery.
Struggling with digestive issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
References
Marshall B. Helicobacter pylori--a Nobel pursuit? Can J Gastroenterol. 2008 Nov;22(11):895-6
Lakhtakia R, Burney I. Self-Experimenting Physicians: Mavericks or martyrs? Sultan Qaboos Univ Med J. 2015 Nov;15(4):e452-5
Watts G. Nobel prize is awarded to doctors who discovered H pylori. BMJ. 2005 Oct 8;331(7520):795
Hooi JKY et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology. 2017 Aug;153(2):420-429
Shatila M, Thomas AS. Current and Future Perspectives in the Diagnosis and Management of Helicobacter pylori Infection. J Clin Med. 2022 Aug 30;11(17)
Öztekin M, Yılmaz B, Ağagündüz D, Capasso R. Overview of Helicobacter pylori Infection: Clinical Features, Treatment, and Nutritional Aspects. Diseases. 2021 Sep 23;9(4):66
Shirin D et al. Real-world Helicobacter pylori diagnosis in patients referred for esophagoduodenoscopy: The gap between guidelines and clinical practice. United European Gastroenterol J. 2016 Dec;4(6):762-769
Kodama M et al. Influence of proton pump inhibitor treatment on Helicobacter pylori stool antigen test. World J Gastroenterol. 2012 Jan 7;18(1):44-8
Satoh K et al. Biopsy sites suitable for the diagnosis of Helicobacter pylori infection and the assessment of the extent of atrophic gastritis. Am J Gastroenterol. 1998 Apr;93(4):569-73
Lash JG, Genta RM. Adherence to the Sydney System guidelines increases the detection of Helicobacter gastritis and intestinal metaplasia in 400738 sets of gastric biopsies. Aliment Pharmacol Ther. 2013 Aug;38(4):424-31.
Liu L, Nahata MC. Treatment of Helicobacter pylori Infection in Patients with Penicillin Allergy. Antibiotics (Basel). 2023 Apr 10;12(4):737
Tshibangu-Kabamba E, Yamaoka Y. Helicobacter pylori infection and antibiotic resistance - from biology to clinical implications. Nat Rev Gastroenterol Hepatol. 2021 Sep;18(9):613-629.
Correa P, Piazuelo MB. The gastric precancerous cascade. J Dig Dis. 2012 Jan;13(1):2-9.
Wang, C., Nishiyama, T., Kikuchi, S. et al. Changing trends in the prevalence of H. pylori infection in Japan (1908–2003): a systematic review and meta-regression analysis of 170,752 individuals. Sci Rep 7, 15491 (2017)
General Disclaimer
Please note that the opinions expressed here are those of Dr Hussenbux and do not necessarily reflect the positions of Buckinghamhsire Healthcare NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.






This is an excellent post. Well done! When I was a G.I. fellow just a few decades ago in Cleveland we were treated with a visit by Barry Marshall, who regaled us of his long journey and search for truth. He was considered a fringe figure in gastroenterology until he proved his critics wrong. I suspect that the Nobel prize he earned likely further contributed to his reputational recovery. And, as a side issue, how many decades were the corkscrew shaped organisms hiding in plain sight on gastric biopsies!
Comprehensive article. Thank you.