ERCP Explained: Why It's Done and What to Expect
The insider's guide to a procedure 90% of patients have never heard of...until they need it!
"Your eyes look yellow."
Mr H stared at his wife across the breakfast table, coffee mug frozen halfway to his lips.
Yellow? He rushed to the bathroom mirror.
She was right! The whites of his eyes had taken on an unmistakable golden tinge.
Within 48 hours, Mr H underwent a CT and MRI scan revealing a mass pressing against his bile duct, backing up bile into his bloodstream.
Over the next few days his skin began to match his eyes…a deep, unsettling yellow leading to awful all body itch.
That's when I first met Mr H in the gastroenterology ward.
I explained the likely diagnosis and plan going forward.
The procedure? ERCP - Endoscopic Retrograde Cholangiopancreatography.
In english, that’s endoscopy of the bile duct.
Using a tiny wire, we navigated upstream against the flow of digestive juices, placed a metal stent to prop open his crushed bile duct, and watched the sudden gush of bile release into the small bowel.
Two weeks later, Mr H’s eyes were white again.
The stent had bought him precious time. He was ready for surgery that could save his life.
If your doctor has mentioned ERCP, you might be feeling overwhelmed by the terminology and the unknown. Here's everything you need to know about this remarkable procedure.
What is ERCP?
ERCP is a specialised procedure that combines a flexible camera (endoscope) with X-ray imaging to examine and treat problems in your bile ducts and pancreatic ducts; essentially the plumbing system that drains your liver, gallbladder, and pancreas.
The procedure uses a special side-viewing duodenoscope, which has its camera positioned at an angle rather than straight ahead. This unique design gives doctors a better view of the major papilla, the small opening where your bile and pancreatic ducts empty into your small intestine.

During ERCP, your doctor guides the endoscope through your mouth, down your throat, through your stomach, and into the first part of your small intestine (duodenum). Once positioned, a thin tube is passed through the scope into your bile duct. Contrast dye is then injected, and X-ray pictures are taken to clearly show the ductal structure and any problems.
Why You Might Need ERCP
Bile Duct Stones (Choledocholithiasis)
Stones can form in your gallbladder and travel to the bile duct, or form directly in the duct itself. When they block bile flow, they cause:
Severe right upper abdominal pain that may radiate to your back
Jaundice – yellowing of skin and eyes due to blocked bile flow
Cholangitis – a serious bile duct infection causing fever, chills, and severe illness requiring urgent treatment
ERCP is particularly effective here, as doctors can use special instruments to extract stones directly.
Biliary Strictures
These are narrowing or blockages of bile ducts caused by:
Cancer of the bile ducts (cholangiocarcinoma) or nearby structures
Scarring from previous inflammation, surgery, or treatments
Inflammatory and autoimmune diseases
External compression from pancreatic cancer or enlarged lymph nodes
Strictures cause similar symptoms to stones, including jaundice and pain (less likely). ERCP allows both diagnosis and treatment through stent placement to keep ducts open.
Understanding the Risks
While generally safe with experienced specialists, ERCP carries more risks than routine endoscopy:
Post-ERCP Pancreatitis
Unfortunately, the pancreas is very close to the bile duct. During the procedure, the pancreas can become irritated leading to pancreatitis
Occurs in 5-10% of procedures
Causes severe abdominal pain, nausea, vomiting
Will require several days of hospitalisation - rarely requires a prolonged admission
Prevention: Your doctor will likely give you rectal anti-inflammatory medication (ibuprofen or diclofenac) before the procedure, significantly reducing this risk
Other Serious Complications
Bleeding: Particularly if a sphincterotomy (small cut) is made
Infection: Of bile ducts or bloodstream
Perforation: A tear in the intestine or bile duct
Though relatively rare, these complications can be severe and potentially life-threatening. This is why ERCP is reserved for situations where benefits clearly outweigh risks; patient discussion prior to the procedure is paramount!
Pre-Procedure Preparation
Pre-Assessment Consultation
The medical team should ideally:
Review your medical history and current medications
Perform a physical examination
Assess whether benefits outweigh risks for your specific situation
Pay special attention if you have heart/lung conditions, previous medication reactions, or kidney/liver problems
Managing Blood Thinners
If you take anti-platelet therapy (clopidogrel, ticagrelor) or anticoagulants (warfarin, (rivaroxaban, apixaban, dabigatran), specific stopping times are required:
Your doctor may arrange temporary bridging if you are at high clot risk
Your trust will have local guidelines which you must adhere to.
If in doubt, mention your medication to your consultant or specialist nurse
Diabetes Management
Special planning includes:
Early morning appointment to minimise eating disruption
Adjusted diabetes medications the evening before and morning of
Bring glucose tablets for potential low blood sugar
Specific instructions from your diabetes team
Your trust will have local guidelines which you must adhere to.
Day of Procedure Requirements
Stop eating and drinking at least 6 hours before
Arrange transportation (no driving for 24 hours post-sedation)
Remove dentures and jewellery
Your trust should provide you with an appropriate patient information leaflet which will provide much more detail
Stent Placement: Critical Information
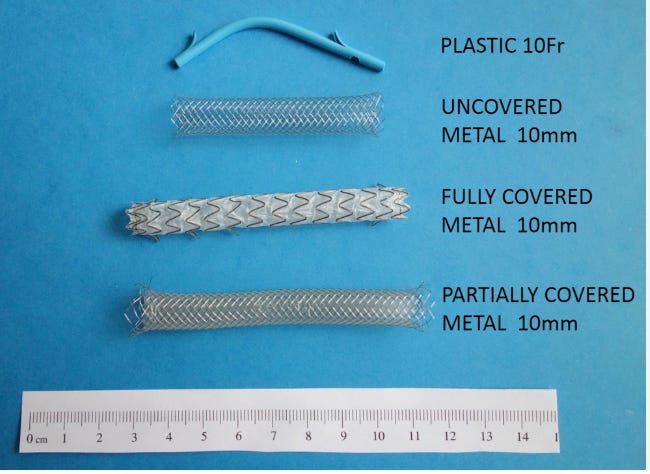
Temporary Stents (Plastic and (sometimes) metal)
Must be removed/replaced within 3-6 months
Used for:
Removing large/multiple stones in stages
Treating bile duct infections
Temporary drainage while planning further treatment
Not removing them can cause serious complications including infection and blockage
Permanent Stents (Metal)
Longer-lasting but still require monitoring
Used for:
Cancer-related strictures
Long-term bile duct narrowing management
Essential: Understand which type you receive; this information will be in your discharge instructions.
Recovery and Aftercare
Normal Recovery Experience
After your ERCP, you will spend a prolonged period in recovery if you received sedation and to monitor for post-ERCP complications.
It is normal to experience some bloating or gas for a few hours after the procedure, and you may have a sore throat that lasts 1-2 days; throat lozenges and salt water gargles can help with this discomfort.
Most people feel well enough to return to work within 2 days.
Important Post-Procedure Restrictions
You cannot drive for 24 hours after sedation, so make sure you have arranged transportation home.
Avoid alcohol for 2 days after the procedure, and don't take blood-thinning medications until your doctor specifically clears you to restart them. This instruction should be written in your endoscopy report.
When to Seek Immediate Medical Attention
Contact your doctor immediately or call 111 (or 911 if in USA) if you experience severe abdominal or chest pain, fever of 38°C or higher, black or tarry stools (which could indicate bleeding), persistent nausea and vomiting, or worsening throat pain or difficulty swallowing. These symptoms could indicate serious complications requiring urgent treatment.
Follow-Up Care
Your medical team will discuss what was found during the procedure and any treatments that were performed. Make sure you understand whether any stents were placed and if they are temporary or permanent, when your next appointment should be scheduled, and whether you need to take any new medications. Having this information clearly documented will help ensure proper ongoing care.
Essential Questions for Your Doctor
Before your procedure:
What specific problem are we looking for or treating?
What are the alternatives to ERCP in my case?
What is your experience with this procedure?
What should I expect for recovery time?
How will the results change my treatment plan?
Conclusion
ERCP is a sophisticated procedure providing both crucial diagnostic information and life-saving treatments for bile duct and pancreatic problems. While it carries risks, when performed by experienced specialists with proper precautions, it's highly effective for conditions that might otherwise cause serious complications.
The key to a successful outcome is being well-informed about what to expect and carefully following all pre- and post-procedure instructions. Remember, this procedure is only recommended when the potential benefits clearly outweigh the risks for your specific condition.
Struggling with digestive issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
References
https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/endoscopic-retrograde-cholangiopancreatography-ercp
https://patient.info/digestive-health/gallstones-and-bile/ercp-endoscopic-retrograde-cholangiopancreatography
https://www.niddk.nih.gov/health-information/diagnostic-tests/endoscopic-retrograde-cholangiopancreatography
Morales SJ, Sampath K, Gardner TB. A Review of Prevention of Post-ERCP Pancreatitis. Gastroenterol Hepatol (N Y). 2018 May;14(5):286-292
Kang X, Xia M, Wang J, et al Rectal diclofenac versus indomethacin for prevention of post-ERCP pancreatitis (DIPPP): a multicentre, double-blind, randomised, controlled trial Gut Published Online First: 20 March 2025.
Grimm IS, Baron TH. Biliary Stents for Palliation of Obstructive Jaundice: Choosing the Superior Endoscopic Management Strategy. Gastroenterology. 2015 Jul;149(1):20-2.
General Disclaimer
Please note that the opinions expressed here are those of Dr Hussenbux and do not necessarily reflect the positions of Buckinghamhsire Healthcare NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.