5 science-backed medications that help with IBS
From 45-minute relief to long-term control: matching the right treatment to your IBS subtype
Welcome back to The Gut Group!
Before I talk about the medications please read this:
https://drhussenbux.substack.com/p/opening-your-mind-to-irritable-bowel
If you want the TLDR:
IBS is common
IBS is a disorder of bowel function rather than structure.
The gut and brain communicate to each other via the enteric nervous system.
The enteric system controls the motility of the bowel (i.e. how fast content moves through the bowel) and pain stimuli.
When there is abnormal communication this can lead to visceral hypersensitivity causing abdominal pain.
Below are five medications that have robust clinical trial evidence for IBS symptoms, but choosing the right one depends on your specific IBS subtype and predominant symptoms. From antispasmodics that work within 45 minutes to gut-brain modulators that re-wire pain processing, these treatments offer genuine relief when first-line approaches like dietary changes aren't enough.
After reviewing thousands of pages of clinical trials and the latest British Society of Gastroenterology guidelines, these five medications stand out for their evidence quality and real-world effectiveness.
What makes this different from typical medication lists is that each has been proven in rigorous randomised controlled trials, with clear guidance on which patients benefit most. The key insight
IBS isn't one condition but several, and matching the right medication to your symptom pattern is crucial for success.
The evidence-based approach transforms IBS treatment
IBS affects 1 in 20 people worldwide, causing abdominal pain and altered bowel habits that significantly impact quality of life. The 2021 British Society of Gastroenterology guidelines ranked treatments based on systematic reviews and network meta-analyses of clinical trials.
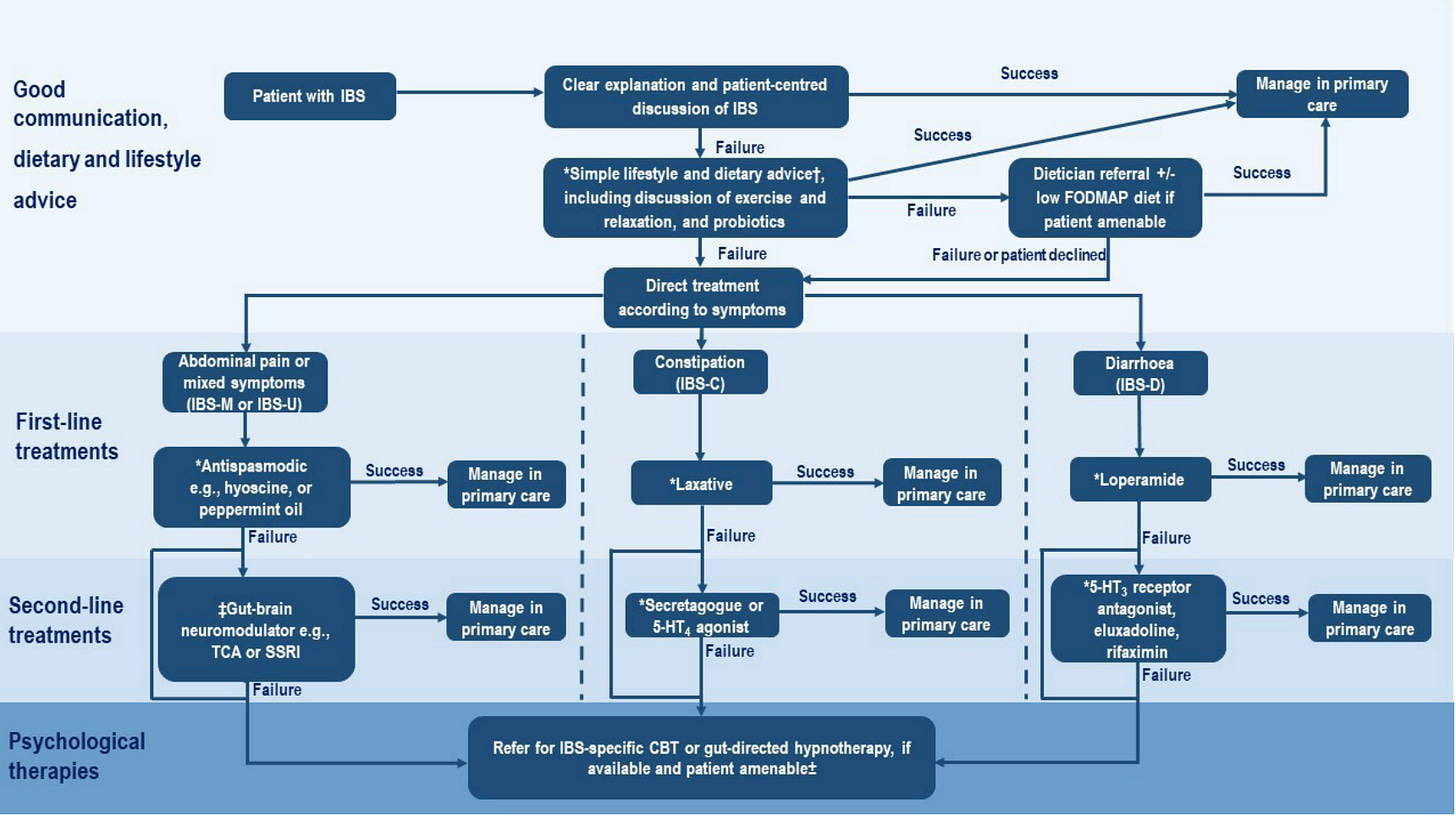
The new evidence hierarchy moves beyond "try this and see" to precision medicine. These five medications each target different aspects of IBS pathophysiology - from smooth muscle spasms to visceral hypersensitivity to gut-brain communication. Understanding their mechanisms helps predict which patients will respond best.
Modern IBS treatment recognises three distinct subtypes: IBS-D (diarrhoea-pre-dominant), IBS-C (constipation-predominant), and IBS-M (mixed pattern). Each responds differently to medications, explaining why generic approaches often fail. The medications below are ordered by strength of evidence and clinical utility.
Important disclaimer: This guide is for people who have already received a formal diagnosis of IBS from a healthcare provider. While some medications discussed are available over-the-counter, others require prescription. Always consult with a healthcare professional before starting any new treatment, and ensure appropriate follow-up to monitor your response and adjust therapy as needed.
1. Peppermint oil delivers rapid symptom relief through calcium channel blockade
The mechanism: L-menthol in peppermint oil blocks calcium channels in intestinal smooth muscle, directly preventing the spasmodic contractions that cause cramping pain.
The evidence: Multiple systematic reviews confirm peppermint oil's efficacy, with the most recent meta-analysis of 12 trials showing a Number Needed to Treat (NNT) of just 4. This means for every 4 patients treated, 1 will experience significant symptom improvement who wouldn't have with placebo. The response rate is typically 58% versus 29% with placebo.
Critical formulation detail: Only enteric-coated capsules work. The coating bypasses stomach acid, delivering therapeutic menthol concentrations to the small intestine and colon where it's needed.
Peppermint tea, despite popular belief, contains insufficient menthol and lacks targeted delivery - no clinical trials support its use for IBS.
Who benefits most: IBS-D and IBS-M patients with predominant cramping pain and bloating. Effects typically begin within 24 hours. The PERSUADE study showed particular benefit for small-intestinal release formulations, with 40% reduction in total IBS symptom scores versus 24% placebo.
Your dose: 180-200mg enteric-coated capsules three times daily, 30-60 minutes before meals. Trial for 4-6 weeks minimum. Can be bought over the counter.
Avoid if you have significant heartburn or gallbladder disease - the menthol can worsen both conditions.
2. Amitriptyline rewires visceral pain processing at doses far below antidepressant levels
The breakthrough research: The ATLANTIS trial, published in The Lancet in 2023, finally provided definitive evidence for low-dose amitriptyline in IBS. This was the largest tricyclic antidepressant study ever conducted in IBS, involving 463 patients across 55 UK general practices.
The mechanism - not what you think: At doses of 10-30mg, amitriptyline works through visceral hypersensitivity modulation, not antidepressant effects. It alters brain-gut pain processing, reducing the exaggerated abdominal pain responses characteristic of IBS. The doses are 3-5 times lower than antidepressant treatment (75-150mg), explaining why mood effects are minimal.
The evidence: ATLANTIS participants taking amitriptyline were almost twice as likely to report overall symptom improvement compared to placebo. The IBS Severity Scoring System showed a 99-point improvement versus 69 points with placebo. Crucially, depression scores didn't change, confirming the mechanism isn't antidepressant-related.
Patient-led dosing innovation: The trial used a novel self-titration approach where patients adjusted their dose based on symptoms and side effects, starting at 10mg and titrating up to 30mg as needed. This personalised approach improved both efficacy and tolerability.
Who benefits most: Moderate-to-severe IBS patients who have failed first-line treatments, particularly those with IBS-D or IBS-M (over 80% of ATLANTIS participants). Average IBS duration in the trial was 10 years, showing effectiveness even in long-standing cases.
Your dose: Start 10mg once daily at bedtime (due to sedating effects). Self-titrate over 3 weeks up to maximum 30mg daily based on response and side effects. Most common side effects are dry mouth (54%) and drowsiness (53%), which typically improve with time. Needs specialist input and follow up.

3. Buscopan provides rapid relief for cramping through targeted muscle relaxation
The mechanism: Hyoscine butylbromide acts as a highly selective muscarinic receptor antagonist, blocking acetylcholine-mediated smooth muscle contractions specifically in the gut. Its key advantage is minimal systemic absorption (less than 1% bioavailability), meaning it works locally without central nervous system effects.
The evidence: A 2008 meta-analysis of 22 trials showed antispasmodics achieve an impressive NNT of 3.5 specifically for hyoscine butylbromide - meaning roughly 1 in 3 patients will experience clinically meaningful improvement. The effect is rapid, with meaningful pain relief occurring within 45 minutes versus 60 minutes for placebo.
The speed advantage: Unlike other IBS medications that require weeks to work, Buscopan provides relief within 30-45 minutes, making it ideal for on-demand use during symptom flares. This rapid onset reflects its direct mechanism on smooth muscle contractions.
Who benefits most: Primarily IBS-D patients with cramping abdominal pain, as the mild constipating effects actually help diarrhoeal symptoms. Studies show it increases rectal pain thresholds significantly, directly addressing the visceral hypersensitivity component of IBS. Can be bought over the counter.
Your dose: 10mg tablets, 1-2 tablets three times daily, or use on-demand (1-2 tablets at symptom onset, can repeat every 30 minutes, maximum 6 tablets daily). Buscopan can be taken 30-60 minutes before meals if postprandial symptoms are prominent. Avoid in IBS-C due to constipating effects.
4. Linaclotide uniquely targets both constipation and abdominal pain through dual cGMP pathways
The dual mechanism breakthrough: Linaclotide is a guanylate cyclase-C agonist that increases both intracellular and extracellular cyclic GMP. Intracellularly, it stimulates chloride secretion and accelerates intestinal transit. Extracellularly, it modulates pain-sensing nerves, directly reducing visceral hypersensitivity - a unique dual action no other IBS medication provides.
The evidence gold standard: Linaclotide received a STRONG recommendation with HIGH certainty evidence in the 2022 American Gastroenterological Association guidelines - the highest grade possible. Multiple Phase 3 trials involving over 4,000 patients demonstrate consistent efficacy, with 12.7-17.4% achieving the FDA composite endpoint versus 3.0-5.6% placebo.
Sustained effectiveness: Unlike some IBS treatments that lose efficacy over time, linaclotide maintains benefits throughout 26-week studies. Abdominal pain improvement occurs in 38.9% versus 19.6% placebo, while complete spontaneous bowel movements increase in 18.1% versus 5.0% placebo.
Who benefits most: Adults with moderate-to-severe IBS-C who need both constipation and abdominal pain relief. This fills a critical treatment gap, as your other medications primarily address IBS-D symptoms. About 35% of IBS patients have constipation-predominant symptoms.
Your dose: 290 micrograms once daily, taken 30 minutes before your first meal of the day on an empty stomach. The most common side effect is diarrhoea (9-20%), usually mild-moderate and occurring early in treatment. Most patients who experience diarrhoea continue treatment as it often resolves. Needs specialist input and follow up.
5. Prucalopride accelerates transit but lacks IBS-specific evidence
The mechanism: Prucalopride is a highly selective 5-HT4 receptor agonist that stimulates acetylcholine release from enteric neurones, promoting coordinated colonic contractions and accelerating intestinal transit. It induces giant migrating contractions - powerful waves that propel contents through the colon.
The evidence gap: Despite robust effectiveness for chronic constipation, prucalopride has no dedicated clinical trials in IBS-C patients. The 2021 American College of Gastroenterology guidelines explicitly recommend against using prucalopride for overall IBS symptoms due to this evidence gap.
Why the distinction matters: IBS-C and chronic constipation aren't the same condition. IBS involves visceral hypersensitivity and abdominal pain, while chronic constipation primarily involves slow transit. Prucalopride may help the constipation component but could potentially worsen abdominal pain in IBS patients.
Current status: While mechanistically plausible for IBS-C, current evidence-based practice recommends proven treatments like linaclotide first-line. Prucalopride might be considered in patients where constipation (despite taking laxatives) with slow transit is suspected.
Your dose (if used off-label): 2mg once daily for adults under 65, reduced to 1mg daily for those over 65 or with renal impairment. Common side effects include headache (25-30%) and nausea (12-24%), usually transient and occurring in the first 1-2 days.
Choosing your optimal medication strategy
The selection algorithm: Start with your IBS subtype. IBS-D patients typically respond best to peppermint oil or Buscopan for immediate relief, with amitriptyline for those needing ongoing symptom control. IBS-C patients should consider linaclotide first-line given its strong evidence base and dual mechanism. IBS-M patients may benefit from peppermint oil or amitriptyline depending on predominant symptoms.
Timing and combinations: These medications can often be used together strategically. For example, peppermint oil or Buscopan for acute symptom flares while building up amitriptyline for long-term control. Always discuss combinations with your healthcare provider to avoid interactions and optimise timing.
When to seek specialist help: If you don't achieve satisfactory improvement with two different evidence-based treatments, or if you develop new concerning symptoms, gastroenterology referral is warranted. Red flag symptoms requiring immediate evaluation include weight loss, rectal bleeding, iron deficiency anaemia, or onset after age 50.
The landscape of IBS treatment has transformed dramatically with these evidence-based options. Rather than suffering through years of trial-and-error, patients now have scientifically validated treatments that target the specific mechanisms driving their symptoms. The key is precision - matching the right medication to your symptom pattern and IBS subtype for optimal outcomes.
Struggling with digestive issues that affect your daily life? Invest in your gut health with a private, personalised consultation where I will explore your specific symptoms and develop a targeted treatment plan. Take the first step toward digestive wellness today: https://bucksgastroenterology.co.uk/contact/
References
Vasant DH et al. British Society of Gastroenterology guidelines on the management of irritable bowel syndrome. Gut. 2021 Jul;70(7):1214-1240
Chang L et al. AGA Clinical Practice Guideline on the Pharmacological Management of Irritable Bowel Syndrome With Constipation. Gastroenterology. 2022 Jul;163(1):118-136.
Lembo A et al. AGA Clinical Practice Guideline on the Pharmacological Management of Irritable Bowel Syndrome With Diarrhea. Gastroenterology. 2022 Jul;163(1):137-151.
Cash B. Novel Peppermint Oil Formulation for Dietary Management of Irritable Bowel Syndrome. Gastroenterol Hepatol (N Y). 2015 Sep;11(9):631-3.
Hawthorn M et al. The actions of peppermint oil and menthol on calcium channel dependent processes in intestinal, neuronal and cardiac preparations. Aliment Pharmacol Ther. 1988 Apr;2(2):101-18.
Alammar N et al. The impact of peppermint oil on the irritable bowel syndrome: a meta-analysis of the pooled clinical data. BMC Complement Altern Med. 2019 Jan 17;19(1):21.
Ingrosso MR et al. Systematic review and meta-analysis: efficacy of peppermint oil in irritable bowel syndrome. Aliment Pharmacol Ther. 2022 Sep;56(6):932-941
Ford AC et al. ATLANTIS trialists. Amitriptyline at Low-Dose and Titrated for Irritable Bowel Syndrome as Second-Line Treatment in primary care (ATLANTIS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2023 Nov 11;402(10414):1773-1785.
Ford AC et al. Effect of fibre, antispasmodics, and peppermint oil in the treatment of irritable bowel syndrome: systematic review and meta-analysis. BMJ. 2008 Nov 13;337:a2313.
Omer A, Quigley EMM. An update on prucalopride in the treatment of chronic constipation. Therap Adv Gastroenterol. 2017 Nov;10(11):877-887.
Quigley EM. Prucalopride: safety, efficacy and potential applications. Therap Adv Gastroenterol. 2012 Jan;5(1):23-30. doi: 10.1177/1756283X11423706
General Disclaimer
Please note that the opinions expressed here are those of Dr Hussenbux and do not necessarily reflect the positions of Buckinghamhsire Healthcare NHS Trust. The advice is intended as general and should not be interpreted as personal clinical advice. If you have problems, please tell your healthcare professional, who will be able to help you.








Thanks for writing about this.
IBS is more than a bothersome digestive issue: it is a chronic, often invisible condition that disrupts physical health, mental well‑being, professional life, and finances.
It urgently needs greater recognition, open discussion, and comprehensive approaches; from awareness and early diagnosis to integrated care, to alleviate its societal burden and restore the quality of life for millions.
This is great stuff! I’m also wondering if you have any knowledge about gallstones and the gallbladder? I would love to see you apply your scientific approach to that topic in a post one of these days.